Chances are good that if you don't suffer from back pain you know someone who does. Most back pain sufferers complain of lower or upper back pain but there is that seldom talked about and elusive middle back pain that gets very little lip service.
The truth is that though we don't hear about it very often, middle back pain is a common source of back pain among manual laborers. While the population as a whole doesn't suffer from mid back pain as much as manual laborers, there are a variety of reasons for your current bout of middle back pain.
Should you be concerned about mid back pain? Quite simply: yes. Because the portion of the back sandwiched between the upper and lower back gets less use, an injury to this portion of the back is incredibly painful and severely limits upper body mobility.
Where Exactly Is Your Mid Back?
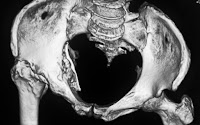
Although some upper and lower back pain radiates up and down, the middle back goes from your shoulders and ends at the base of the rib cage. The pain will be more concentrated in this area than it is when you suffer from other forms of pain in the back.
What Causes Mid Back Pain?
Unlike the other forms of back pain, middle back pain doesn't have quite as many causes. While injury can cause just about any type of back pain, there are a few common causes, including:
- Poor posture Thanks to too many hours spent in front of computer screens, tablets and e-readers, middle back pain is due to that weird hunch associated with technology hounds.
- Trauma is a common cause of back pain whether due to a fall, a football hit, auto accident or improper lifting.
- Bad sleep posture isn't something we often think of as a source for back pain, but the truth is how we sleep for hours at a time can have a serious impact on the middle back area. Sleeping (or standing) hunched over has the same impact as sitting hunched over a computer screen.
- Excess weight causes many types of back pain because it strains the muscles in the back, causing pain. Specifically an excessively large stomach can pull at the lower and middle back, causing muscle strain.
Symptoms
How do you know if that nagging pain in the middle of your back is a simple run-of-the-mill backache or actual middle back pain? It can be difficult to tell the difference since you won't feel that unbearable pain associated with lower back pain and because the mid-back muscles get used far less.
The most obvious symptom of middle back pain is a limited range of motion particularly when bending. If you bend beyond what the pain allows, it may be dull or sharp pain radiating throughout the midsection of the back. Sometimes the pain can be accompanied by numbness or tingling, especially after long periods of inactivity.
It will be very hard to know if your pain is more than a simple ache, but that is why it is important to seek out a back specialist. You need to make sure that a few days of pain don't turn into several weeks or months, allowing the pain and your range of motion to worsen.
An Ounce of Prevention...
If you've ever suffered from any type of back pain in the past and wished you could have done something to prevent it, the good news is that you can. In fact, simple acts such as regular exercise and a healthy diet can go a long way to help prevent muscle strain in the middle back. Exercise keeps the muscles strong and when combined with a healthy diet, is conducive to weight loss, which will reduce muscle strain.
Do you spend time staring in the mirror at the gym while you pump iron? If so you may want to take it easy and reduce the weight on your bar. Often the problem is simply that we're trying to push our bodies further than its ready to go. This happens often with those who are returning to exercise after a long period of inactivity or those trying to expedite their weight lifting goals.
The moment you begin to notice pain in the middle back you should reduce the weight you're lifting. In general, however, if you feel that you are having difficulty with a heavier weight, reduce it.
One of the best prevention tools for mid back pain is ergonomic equipment. Use ergonomic keyboards, desks and office chairs to keep your back properly aligned. If you need a sleep pillow to keep your posture proper in sleep, there are many places to purchase one to stop mid back pain before it starts.
Rest your body properly after any amount of physical exertion. Muscle strain can turn into a long-term problem if you continue to push your body too far and the best way to prevent it is to let your body rest. Whether it is after a workout, a long day of manual labor or sitting at a desk, take a few minutes to stretch and relax your muscles.
Slow Burn
Middle back pain is a problem that takes time before you truly begin to experience painful or uncomfortable symptoms. This is why you should take note of your symptoms as they pop up and if the pain persists for longer than a couple of weeks, get in to see your doctor immediately.
The sooner you take care of the pain in the early stages, the less likely it is to make it to the more painful stages.